Featured News
Effects of Boxing on Testosterone Levels
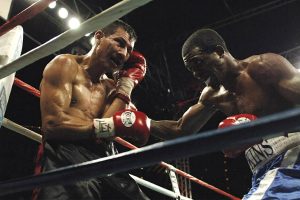
Boxing is an aerobic form of exercise that is rigorous and demanding. In general, boxing has both physical and mental benefits. This exercise is believed to aid in boosting testosterone levels. But is this true, and do all boxers have naturally high testosterone levels, or do some boxers take legal steroids? Let us find out how boxing affects the levels of testosterone. How Boxing Affects Testosterone Levels Naturally, men who have an active and good physical condition are more likely to have higher testosterone levels …

What Athletes Should Know Before Using CBD
Many athletes today put their bodies under too much physical exercise. Many positive effects result from athletes exercising, such as increased performances and muscle adaptation – Click here to learn more. However, exercise also has adverse effects, such as wear and tear of the muscles and trauma. Due to the pain, athletes rely on other ways to manage dangerous pain, which can lead to death. This process has led many athletes to question whether CBD is safer for relieving excess pain. The use of extra …

Can CBD Oil Help Professional Boxers Recuperate Faster?
Boxers enter the ring expecting they would, at the very least, take a few blows. They are well aware that they are in it to win it. As a result, the sport impacts the physical and the psyche. CBDNorth’s gummies are a brand-new and eye-catching method to take CBD. Before professional boxers can return to the ring, they must recover from the hit, which causes bruises, swelling, and agony. CBD oil in Canada, and other forms of CBD, have made their way into the professional …

Vaping And Athletes: What You Need To Know
Athletes have always been associated with healthy habits, a good green diet with lots of proteins & essential vitamins, articles pour vapoteurs montreal and fit athletic bodies. They are always asked to stay away from any unhealthy habits which might impact their health and performance. Thus, smoking is a big no-no for them. But, what about vaping? If you are wondering whether vaping is good or bad for athletes, then you are on the right page. Continue reading below to get essential information that will …







